Medical research is one of the most important outputs for a university, with breakthroughs potentially saving lives around the world. Professor Stephen Gillespie and colleagues at the School of Medicine have done just this, developing global capacity to improve tuberculosis treatment by developing shorter, safer drug regimens, and improved diagnostics for monitoring treatment.
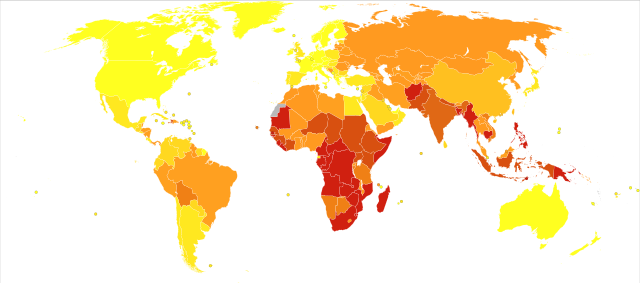
Tuberculosis (TB) is a major global killer with approximately 9 million new cases and 1 million to 2 million deaths per year, disproportionally affecting low and middle-income countries. The School of Medicine has researched the disease, and the pathogen responsible for it, for the last decade, contributing to transformative changes in how TB is tackled around the world. These have encompassed the development of global TB networks, new treatment methods and increased clinical capacity. The research has improved diagnostics for monitoring treatment, which led to the development of a tool to monitor antibiotic treatment of TB patients in real time.
The foundation of their research involved conducting the first clinical trials for a selection of new and repurposed drugs. To achieve this, the group formed a series of international collaborations across Africa, South Asia, Europe and South America. With these consortia, the School carried out REMoxTB, the first regulatory study of the drug moxifloxacin as part of a TB treatment regimen, across nearly 50 sites in Africa and Asia.
REMoxTB began the team’s longstanding project to develop global capacity to improve tuberculosis treatment. Subsequent steps included the establishment of trial sites in Africa, Asia and South America to run therapeutic and diagnostic projects. These projects also addressed critical questions in tuberculosis management including the understanding of the toxicity of tuberculosis chemotherapy, especially regarding liver injury, the differing effectiveness of treatment across gender, and how to interpret positive blood culture tests after patients have completed therapy. The progress of the research has resulted in two further regulatory trials in collaboration with the Global Alliance for TB Drug Development. The first, STAND, was completed in 2018 and published recently; the second, SimpliciTB, began the same year and is currently ongoing.
In addition to regulatory trials, the Infection and Global Health group has made great strides in repurposing and optimising existing drugs. Gillespie is one of the three leads in the PanACEA consortium, one of the international tuberculosis research associations established in part by the School, which has performed a series of early phase trials. These include a process to determine the optimal dose of rifampicin, an antibiotic administered to treat tuberculosis which is the most important component of the current treatment regimen. This research has demonstrated the antibiotic’s effectiveness at killing TB bacteria and determined its optimum dose.
Aside from treatment itself, another critical barrier to the effective management and treatment of tuberculosis is diagnosing the disease and monitoring patient response during treatment. The diagnosis is especially crucial, given that the infecting bacteria grow very slowly and hence an early diagnosis can significantly increase survival rate. In response, the group developed a test known as the Tuberculosis Molecular Bacterial Load Assay TB-(MBLA), which not only diagnoses the disease definitively but can also determine whether the TB pathogen is alive or dead, allowing clinicians to monitor the patient’s response to treatment and adjust it accordingly. It has also significantly reduced the diagnosis timescale to just four hours, allowing for more up-to-date assessments of patient recovery. The TB-MBLA is now used in research laboratories in 16 countries across the world, with over 40 researchers and practitioners from Africa, Asia and Europe trained in its use. The team aims to have reached all ODA countries with a high TB burden by 2025.
The TB-MBLA was developed in Prof Gillespie’s laboratory, and the international evaluation study was led by Dr Wilber Sabiiti. The team has also assisted in the development of the Holistic Approach to Unravel Antibacterial Resistance in East Africa (HATUA). Led by Professor Matthew Holden, the project aims to tackle a problem that, by 2050, is predicted to cost 10 million lives and 100 trillion US Dollars worldwide each year. An interdisciplinary study, HATUA explores biological, socioeconomic, and behavioural drivers of antibacterial resistance in the East African context, but is generalisable to the rest of the world. The project enrolled nearly 2,000 UTI positive patients from 9 study areas across Uganda, Kenya and Tanzania, and the preliminary findings show a complex interplay of factors and pathways in how people seek healthcare and use antibiotics that has great potential for future research.